A new antibiotic could zap super gonorrhoea, a treatment-resistant strain of the STI which is increasing in the UK.
Gepotidacin, which is taken as a pill, is already used to treat urinary tract infections.
Now it could be prescribed for gonorrhoea too – which is good news, given that the UK Health Security Agency warned last month that resistance could make it ‘untreatable’ with traditional methods.
The unpleasant disease is one of the oldest sexually transmitted infections, and the second most common in the UK.
Even the ancient Greeks were worried about it, and its name means ‘an unwanted discharge of semen’, which mistakenly refers to the pus it can cause.
A new study published in The Lancet compared gepotidacin with the current standard treatment in 628 patients.
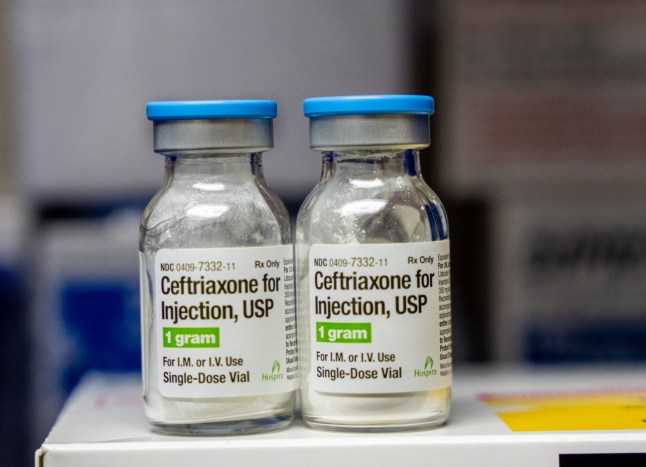
Experts found that the new pill is as effective as the current standard treatment, ceftriaxone with azithromycin, for treating the infection.
It was also found to be able to treat strains that were resistant to current first-line treatments.
What is gonorrhoea?
Caused by infection with the Neisseria gonorrhoeae bacteria, it is primarily spread by vaginal, oral or anal sex.
Symptoms include unusual discharge from the penis or vagina, pain or burn when urinating, itching, bleeding and soreness, and can affect the genitals, rectum, and throat,
Left untreated, gonorrhoea can cause infertility in men and women, and if babies are born with it from an infected mother, they can even become blind.
Most cases begin with no symptoms, however, illustrating the important of testing.

What is the new antibiotic for it?
Researchers said: ‘Gepotidacin is a novel oral antibacterial treatment with the potential to become an alternative option for the treatment of gonococcal infections.’
It works by stopping the bacteria from replicating, effectively killing it.
Antibiotics don’t all work in the same way. They have a variety of mechanisms to defeat micro-invaders, such as destroying their cell wall, or stopping them making proteins they need to survive.
What other treatments are available?
As there is not yet any vaccine for the disease, we rely on treating it once it is contracted.
The antiobiotic ceftriaxone is given with azithromycin as a first treatment, but some bacteria are now resistant to this, and while there are other antibiotic options, they are limited.
Reassuringly, there has been another recent breakthrough in treating the illness.
Zoliflodacin was also shown to successfully neutralise the infection, and was described as a ‘potential game changer for sexual health’.
Dr Edward W Hook III, protocol chair for the study, said it could ‘simplify gonorrhoea therapy for clinicians worldwide.’
But laboratory tests showed the bacteria can still evolve resistance to zoliflodacin, and so the drug is being developed only as a treatment for STIs and will not be used to treat other diseases.
Is super gonorrhoea spreading in the UK?
Most cases are still plain old normal gonorrhoea.
But yes, there has been an increase in treatment-resistant cases, where the bacteria keeps on multiplying even after a patient is given standard antibiotics.
Some cases are also classed as ‘extensively drug resistant’ – or XDR – meaning the infection did not respond to ceftriaxone or the second line of treatment.
UKHSA stats on super gonorrhoea
Government figures show that in the 15 months from January 2024 to March 2025, there were 17 cases of ceftriaxone-resistant gonorrhoea. Thirteen were reported in 2024, with four cases in 2025 so far.
This is compared to 16 cases across all of 2022 and 2023.
In the most recent period, there were also nine XDR cases reported of the most resistant strain: six in 2024 and three in 2025 so far.
This is compared to just five cases between 2022 and 2023.
Ceftriaxone-resistant gonorrhoea was first detected in England in 2015 and 42 cases have since been reported.
The UKHSA said that there were about 54,965 gonorrhoea diagnoses at sexual health services in the first nine months of 2024 compared to more than 85,000 in the whole of 2023.
Get in touch with our news team by emailing us at webnews@metro.co.uk.
For more stories like this, check our news page.